Topical steroids can cause atrophy of the skin as a side effect. The skin consists of epidermis and dermis. The epidermis as an outer layer is about 0.2mm in thickness which is very thin. The atrophy of the dermis can be identified as roughness to a certain extent with the naked eye. However, can one identify the atrophy of epidermis with the naked eye?
Before discussing the matter, I describe the histological structure of the epidermis. What provides the thickness of epidermis is Stratum spinosum which consists of 5-10 cell layers. When the number of cell layers decreases, the epidermis becomes atrophic. When it increases, the epidermis becomes hypertrophic. Above it exists Granular layer which consists of 2-3 cell layers. When it decreases or disappears, or when the blue-stained nuclei remain in the Stratum corneum over the Granular layer (parakeratosis), the skin is insufficiently keratinized and functionally defective.
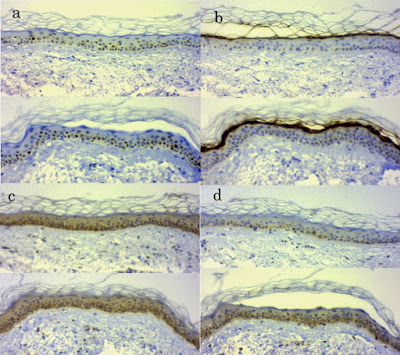
Here is a question. The following six photos of the elbows of different patients contain two atrophic epidermis and two severe insufficient keratinization. Can you identify which they are?
The following is the answer. Stop proceeding to read for a while if you like to think by yourself first.
☆ーーーー☆ーーーー☆ーーーー☆ーーーー☆ーーーー☆
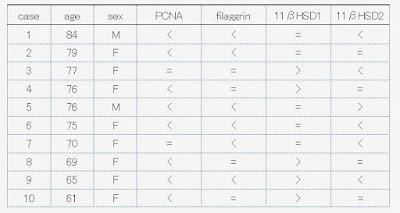
The following is HE stain (left) and anti-cortisol antibody stain (right) of the six patients.
The first and the second patients are topical steroid users. The other four patients have withdrawn from topical steroids. The atrophy of epidermis can be seen in the first and fifth cases and the hypertrophy of epidermis in the third, fourth and sixth cases. Severe insufficiency of keratinization can be seen in the third and fourth cases.
Though the patients are different, the photos are arranged according to the stage of the disease. The first patient is using topical steroids. Though the appearance of the skin is normal, the epidermis is atrophic histologically. The second patient is just unable to control by topical steroids and anti-cortisol staining of the epidermis revealed that there are obvious patty defects. The third and fourth are in the situation that hypertrophy and insufficient keratinization of the epidermis are prominent. They are on rebound which has been prolonged. The fifth has withdrawn from topical steroids but is easy to develop eczema even by a subtle stimulation as an aftermath or because of the natively thin skin. The sixth is normal in keratinization though the epidermis is hypertrophic. It is important to seek for any aggravating factor because allergic reaction to something might exist for a long time.
The clinical appearance looks like the process of withdrawal from topical steroids by arranging the photos from the left to the right though the photos are of different patients.
It is right that the epidermis is thin and its atrophy can’t be identified by the naked eye. However, it might be possible to discriminate to a certain extent by the disease phase in fact.
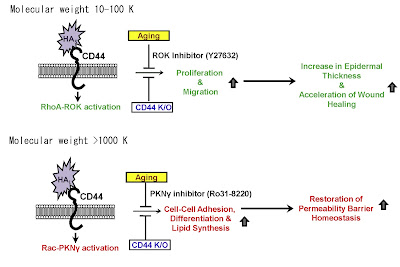
By the way, there are materials which regulate the thickness and differentiation of the epidermis. They are hyaluronic acid with intermediary molecular weight of around 100K Da and that with high molecular weight of over one million Da.
(Bourguignon et al. J Dermatol Sci. 2013 Oct;72(1):32-44. https://www.ncbi.nlm.nih.gov/pubmed/23790635)
Corticosteroids (cortisol) also regulate the thickness and differentiation of the epidermis. Moreover, aging also makes the keratinocyte atrophic.
Three factors to regulate the thickness and differentiation of the epidermis
・Hyaluronic acid ( produced by keratinocyte itself, or topically applied)
・Cortisol ( produced by keratinocyte itself, or topically applied)
・Aging
These three factors are intertwined. Though aging decreases the production of cortisol in keratinocytes, the thickness of the epidermis never increases by it and rather decreases. The atrophy of the epidermis due to topical steroids is competed with hyaluronic acid with intermediary molecular weight.
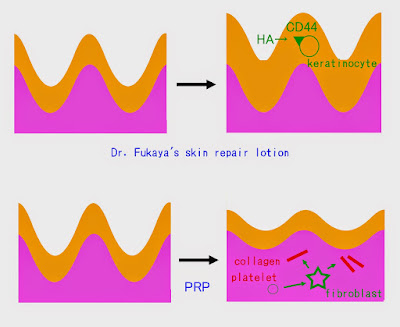
Therefore it must be helpful to apply intermediary-sized hyaluronic acid to epidermal atrophy and high molecular weight hyaluronic acid to insufficient keratinization even if hyaluronic acid itself has no ability to induce cortisol production by keratinocytes.
As there was no available lotion containing hyaluronic acid with around 100k Da which is an intermediary molecular weight in Japan, I commercialized it as a cosmetics naming “Hyaluprotect”.
Though there are many available cosmetics containing hyaluronic acid with high molecular weight in Japan, there is no product disclosing its density. As hyaluronic acid is rather an expensive material, most of them compensate the viscosity by glycerol.
So I tentatively commercialized 1% aqueous solution of hyaluronic acid with a high molecular weight (two million Da) naming as “Hyaluprotect 200”. As there were considerable patients who preferred Hyaluprotect 200, I decided to manufacture a large bottle containing 150 ml.
The most rational way to select the lotion is confirming the status of epidermis by skin biopsy. In cases of above six patients, the first and the fifth cases with atrophic epidermis are suited to Hyaluprotect while the third and the fourth with prominent insufficiency of keratinization are suited to Hyaluprotect 200.
I will offer five 30ml bottles at the same price as the 150 ml bottle until the large bottles are available. For new customers, I recommend trying one by one of Hyaluprotect and Hyaluprotect 200 referring to the above photos (Remember that they are only a suggestion.) You can use both at the same time.
(2016/09/06)
Sorry, the comment column is not available now. But the author believes readers can find some suggestion to overcome their own situations by the previous comments.